Exosomes for Skin Rejuvenation
A review of dermatological applications of exosomes derived from Mesenchymal stem cells, Adipose Tissue and Human Platelet extract
Author: Carolyn Candido, MD (Learn Skin Primary Care Board Member)
Introduction
Over the past decade, breakthroughs in stem cell research and associated cell signaling have illuminated new therapeutic possibilities by harnessing the body’s intrinsic regenerative mechanisms. Aesthetic medicine has particularly benefited from these discoveries, with innovative treatments such as biostimulatory injectable fillers, platelet-rich plasma (PRP), and adipose-derived stem cells becoming increasingly prevalent. These technologies have demonstrated potential in enhancing skin recovery and rejuvenation, though challenges such as variability in preparation and outcomes persist.
Background
Among the latest advancements, exosome-based therapies have emerged as a notable innovation. Exosomes, extracellular vesicles ranging from 30 to 250 nm in diameter, are instrumental in intracellular communication, wound healing, and cellular reprogramming. They carry proteins and nucleic acids that are protected from degradation, and their effects on recipient cells are influenced by their content and the specific receptors on target cells.
The application of exosomes as therapeutic biologics has many advantages over using stem cell therapy. Firstly, exosomes can be stored and transported at low temperatures for a longer duration without significant loss in bioactivity than whole cells. Secondly, exosomes have better penetrating abilities to cross biological barriers and their lipid bilayer membranes can protect the bioactivity of content molecules. Thirdly, exosomes can be quantitatively administered to patients to obtain better clinical effects. Lastly, they are safer than cell transplantation therapy, with less risk of neoplastic transformation and immune response activation.
This makes exosomes a promising tool in aesthetic medicine, for daily topical use and post procedure when used in conjunction with microneedling to enhance skin quality. This review aims to provide a comprehensive overview of the current evidence on adipose, mesenchymal and platelet exosome-based therapies for skin rejuvenation and facial aging. By integrating recent findings and clinical outcomes, we seek to evaluate the transformative potential of exosomes in dermatological treatments and their role in advancing aesthetic medicine.
MSC-Derived Cytokines
MSCs have the ability to differentiate in different types of cells and control the healing response by releasing cellular chemical messengers called cytokines. Mesenchymal stem cells (MSCs) have therapeutic potential on skin wound healing and regeneration, exosomes derived from MSCs have been shown to promote the proliferation and migration of epithelial cells and fibroblasts. Exosomes have demonstrated positive results for wound healing and skin regeneration, indicating that using these exosomes can serve as a replacement treatment for whole-cell therapy with mesenchymal stem cells. (Hu, 2022).
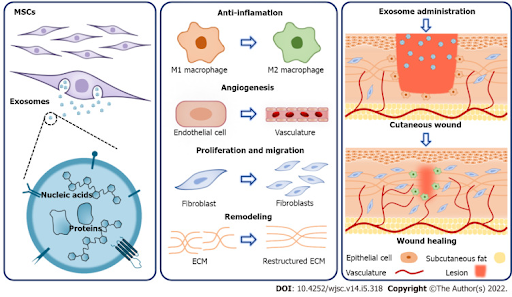
Figure 1. Mechanisms underlying the therapeutic effects of mesenchymal stem cell-derived exosomes on cutaneous wound healing. Mesenchymal stem cell (MSC)-derived exosomes contain a variety of proteins and nucleic acids and hold great potential for promoting cutaneous wound healing. Specifically, MSC-derived exosomes exert therapeutic effects through multiple mechanisms. They can inhibit inflammation via modulating macrophage polarization. Besides, during the proliferation phase, MSC-exosomes promote angiogenesis, as well as the proliferation and migration of fibroblasts. Furthermore, MSC-exosomes can improve extracellular matrix remodeling. As a result, MSC-derived exosomes have offered a new paradigm in the treatment of cutaneous wounds. ECM: Extracellular matrix; MSC: Mesenchymal stem cell.
A promising application of MSC exosomes in anti-aging is by stimulating the rejuvenation of human skin. Exosomes derived from human umbilical cord blood mesenchymal stem cells were tested on human skin tissues by (Kim, 2017). They discovered that exosomes were absorbed by the epidermis after 18 h and lead to increased collagen I and elastin expression levels in human skin after 3 days of treatment (Kim, 2017).
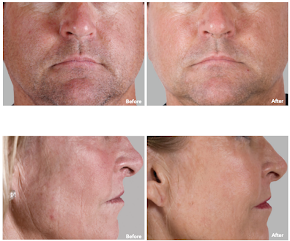
In another study conducted by AnteAGE®, demonstrated clinical efficacy of cytokines derived from adult mesenchymal stem cells of bone marrow origin, incorporated into a facial skin care serum. The clinical trial (n=48) confirmed previous findings that MSC-derived cytokines significantly and rapidly improve skin appearance in patients aged 30 to 75 years old. The treatment led to noticeable enhancements in rosacea, age spots, and fine lines and wrinkles, 85% saw improvement in 6 or more criteria; 61% saw improvement in 9 or more criteria; 32% saw improvement in all 12 criteria with continued use showing potential for further improvement and protection against the adverse effects of aging.
Adipose Tissue stem cell-derived exosomes
Adipose tissue-derived stem cells (ADSCs) have been shown to promote fibroblast proliferation and collagen synthesis, accelerate extracellular matrix remodeling, and increase dermal thickness. ADSC derived exosomes were shown to be taken up by fibroblasts, increases in cell proliferation and migration compared to the behavior of cells without exosome treatment. More importantly, both the mRNA and protein levels of type I collagen (Col 1), type III collagen (Col 3), MMP1, bFGF, and TGF-β1 were increased in fibroblasts ((Zhang, 2018).
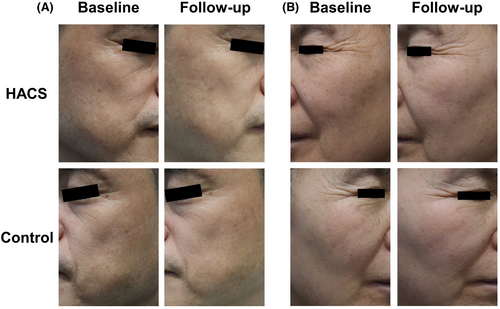
In a recent study, microneedling was used to facilitate ASCE penetration into the dermis, highlighting the efficacy of adipose tissue stem cell-derived exosomes (ASCEs) in treating facial skin aging when combined with microneedling. A recent 12-week, prospective, randomized, split-face study (n=28) demonstrated significant improvements in skin wrinkles, elasticity, hydration, and pigmentation with the application of ASCE-containing solutions combined with microneedling. This approach not only showcased enhanced clinical outcomes but also underscored the safety and effectiveness of exosome-based therapies (Park, 2023).
Figure 3. Baseline and follow-up photographs of the HACS and control sides in (A) a 52-year-old male (GAIS scores of 5 and 3, respectively) and (B) a 60-year-old female (GAIS scores of 5 and 4 respectively). HACS: human adipose tissue stem cell-derived exosome-containing solution; GAIS: Global Aesthetic Improvement Scale.
Platelet Derived Exosomes
Platelets are the first responders in wound-healing cascade, containing endogenous growth factors and signaling molecules to enhance skin renewal. Human Platelet extract (HPE) is an allogenic exosome product derived from US sources, leukocyte-reduced apheresed platelets, offering consistent and potent solutions for skin rejuvenation. A recent study investigated the safety and efficacy of HPE on skin rejuvenation over in prospective, single-arm, non-randomized, longitudinal study over 6 weeks (n=56) (Proffer, 2022). The study underscored the potential of a topically applied platelet-derived exosome product (HPE) to address the signs of aging. Key findings included improvement in redness, wrinkles, and melanin production (P=0.005, P=0.0023, P<0.0001), in addition to improvement in luminosity and color evenness (P<0.001). The topical formulation of Human Platelet extract (HPE) has the potential to have superior results due to its consistency and potency compared with commercially available PRP systems with platelet concentration variability and short half life. (Proffer, 2022).
Skin Cancer and Exosomes
For patients with a history of skin cancer in remission, the use of exosomes, whether as part of a treatment regimen or for other purposes, requires careful consideration. While exosome therapy is an exciting area of research, several potential contraindications and concerns must be addressed, particularly for individuals in remission:
Risk of Recurrence: Exosomes can carry various molecular signals, including growth factors and genetic material. In patients in remission, there is a risk that exosomes could inadvertently contribute to tumor recurrence or progression, particularly if they contain factors that stimulate dormant cancer cells.
Immune System Interaction: Exosomes can modulate immune responses. For patients in remission, maintaining a robust immune system is crucial to preventing cancer recurrence. If exosomes have immunomodulatory effects, they could potentially impact the immune surveillance needed to detect and eliminate residual cancer cells.
Potential for Tumor-Promoting Factors: Exosomes might contain or influence the release of molecules that could support tumor growth. Even if the patient is in remission, there is a risk that these factors might activate residual cancer cells or create a microenvironment conducive to relapse.
Interactions with Other Treatments: Patients in remission might be on maintenance therapies or follow-up treatments to prevent recurrence. The interaction between exosome therapies and these existing treatments needs to be understood to avoid potential negative effects or reduced efficacy.
Safety Profile: The long-term safety profile of exosome-based therapies is not fully established. For patients in remission, the potential for unexpected adverse effects or complications must be thoroughly evaluated.
Monitoring and Follow-Up: If exosome therapy is considered, close monitoring is necessary to promptly detect any signs of recurrence or adverse effects. Regular follow-up and surveillance are crucial for patients with a history of cancer.
Regulatory and Ethical Concerns: The use of exosomes must comply with ethical guidelines and regulatory requirements. This includes ensuring that any exosome-based therapies are approved and that their use in patients with a history of cancer is supported by clinical evidence.
Discussion
Exosomes have demonstrated promising results in improving skin appearance, offering significant benefits for aging skin. These results align with the trend of integrating innovative treatments into dermatological practice, reflecting a shift towards therapies that address both aesthetic and functional aspects of skin health. While exosome-based therapies have applications in aesthetics and regenerative medicine, their use in patients with a history of skin cancer in remission requires careful consideration of these factors.
References
1 Casado-Díaz, A., Quesada-Gómez, J. M., & Dorado, G. (2020). Extracellular Vesicles Derived From Mesenchymal Stem Cells (MSC) in Regenerative Medicine: Applications in Skin Wound Healing. Frontiers in bioengineering and biotechnology, 8, 146. https://doi.org/10.3389/fbioe.2020.00146
2 Hu JC, Zheng CX, Sui BD, Liu WJ, Jin Y. Mesenchymal stem cell-derived exosomes: A novel and potential remedy for cutaneous wound healing and regeneration. World J Stem Cells. 2022 May 26;14(5):318-329. doi: 10.4252/wjsc.v14.i5.318. PMID: 35722196; PMCID: PMC9157601.
3 Kim YJ, Yoo SM, Park HH, Lim HJ, Kim YL, Lee S, Seo KW, Kang KS. Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulates rejuvenation of human skin. Biochem Biophys Res Commun. 2017 Nov 18;493(2):1102-1108. doi: 10.1016/j.bbrc.2017.09.056. Epub 2017 Sep 14. PMID: 28919421.
4 Park, G. H., Kwon, H. H., Seok, J., Yang, S. H., Lee, J., Park, B. C., Shin, E., & Park, K. Y. (2023). Efficacy of combined treatment with human adipose tissue stem cell-derived exosome-containing solution and microneedling for facial skin aging: A 12-week prospective, randomized, split-face study. Journal of cosmetic dermatology, 22(12), 3418–3426. https://doi.org/10.1111/jocd.15872
5 Proffer, S. L., Paradise, C. R., DeGrazia, E., Halaas, Y., Durairaj, K. K., Somenek, M., Sivly, A., Boon, A. J., Behfar, A., & Wyles, S. P. (2022). Efficacy and Tolerability of Topical Platelet Exosomes for Skin Rejuvenation: Six-Week Results. Aesthetic surgery journal, 42(10), 1185–1193. https://doi.org/10.1093/asj/sjac149
Comments


0 Comments